Lindsey Waddell is a native of Louisville, Kentucky and graduated from the University of Louisville School of Nursing with her BSN and Vanderbilt University School of Nursing with her MSN. She has been providing nursing care to the Nashville community since 2005 and has worked in multiple areas gaining valuable experience in management of medical comorbidities across the lifespan. She has also held multiple management positions gaining experience with organization and employee management. Currently she works for Integumetrix as a Wound Care Consultant. Lindsey brings valuable experience as a nursing educator to Integumetrix. She has held multiple faculty, lecture, and instructor positions in baccalaureate nursing education during her career with specialty areas including Health Assessment and Community Health. Currently she is the primary nurse practitioner for wound care at a level 2 trauma hospital in Nashville, TN.
Waddell_Innovations in Addressing Non-Viable Tissue_2018_Volume 1_Issue 1
BACKGROUND
Recently, Agarwal1 discussed risk factors that can affect all types of surgical subspecialties, and subsequently, the difficulty involved with healing surgical incisions/wounds that follow. The most common of those risk factors are diabetes mellitus, obesity, tobacco use and prolonged surgical time. Impaired wound healing can cause surgical incisions/wounds to have varying amounts of non-viable tissue.
When reviewing current up-to-date treatment modalities for removal of nonviable tissue when surgical debridement is not possible or appropriate, the use of V.A.C. VERAFLO™ Therapy using V.A.C. VERAFLO CLEANSE CHOICE™ Dressing should be considered. A recent retrospective study by Teot et al2reported on preliminary evidence suggesting that the adjunctive use of V.A.C. VERAFLO™ Therapy with V.A.C. VERAFLO CLEANSE CHOICE™ Dressings may be suitable for wound cleansing in chronic, complex wounds when complete surgical debridement is not possible or appropriate.
CLINICAL CASE
Back in late summer, I had the opportunity to work with a 55-year-old Caucasian female who was involved in a motor vehicle accident (MVA) in which her extensive injuries were treated at a level 2 trauma center in June of 2017. As it would turn out, on her third hospital admission the wound care team would be consulted and their clinical services would be utilized for wound complications to the right Gracilis Flap donor site. She sustained multiple injuries to bilateral lower extremities and because of the accident, required extensive surgical intervention.
Her initial hospitalization was 20 days. During this stay, the management of wound care was overseen by the trauma, plastics, and orthopedic services teams. Upon discharge, her diagnosis was as follows: open right ankle fracture dislocation, left ankle fracture, right 5 and 6 rib fractures, bilateral pulmonary contusion, abdominal wall contusion, morbid obesity, chronic pain syndrome, motor vehicle collision, vaginal candidiasis, urinary retention, acute renal insufficiency, chronic narcotic use secondary to pain management issues, hepatitis C and history of bipolar disorder.
Procedures performed by the overseeing services during the first hospitalization included irrigation and debridement of a right open ankle wound, followed by V.A.C.® Therapy and short leg splints to bilateral lower extremities. On day 1 of hospitalization, the following procedures were performed: open reduction and internal fixation of the left medial malleolus for provisional stabilization of the medial malleolus, short leg splint to the right lower extremity and closed reduction and short leg splint to the left lower extremity. An inferior vena cava filter placement occurred on day 2 of hospitalization. Then lastly, on day 13 of hospitalization, she had sharp excisional debridement of an open fracture dislocation of the right ankle. A muscle flap graft was then used to cover the medial portion of the right ankle with exposed structures and hardware. The split-thickness skin graft (STSG) was placed over the Gracilis Flap recipient site to the right ankle. The patient went on to be discharged in late June, 2017 and subsequently returned for 2 additional in-patient hospitalizations related to complications and wound infection.
The second hospitalization was in July 2017 and lasted 5 days when the patient was admitted for a urinary tract infection (UTI) and wound infection to the right medial thigh Gracilis Flap donor site. She was taken to the trauma operating room (OR) for debridement. She was discharged and would return again for another 8 day patient stay later in July (3rd inpatient stay). The diagnosis for this visit included: complications of STSG, necrosis of surgical site, status post MVA with multiple injuries, infection of the right leg donor site, leukocytosis, anemia and morbid obesity. The wound care team was consulted after debridement of the Gracilis Flap donor site wound performed by trauma, after which V.A.C.® therapy was initiated.
TREATMENT APPROACH AND FOLLOW-UP
According to Philippe-Gouin and Kiecolt,3 psychological stress may lead to clinically relevant delays in wound healing. The authors suggested that the relationship between stress and wound repair is not only significant, but also clinically relevant.
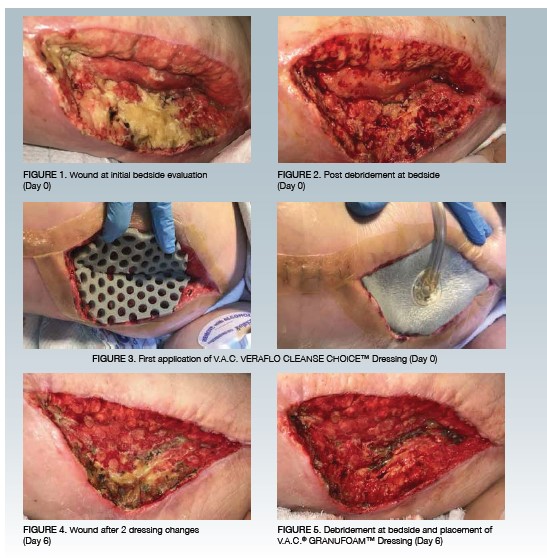
The patient whose condition is described above and for whom I was about to care for was extremely stressed. She told me that she was physically, emotionally and mentally worn out from repeat hospitalizations and surgical interventions. Upon entering the room for the first time to meet the patient, she began crying and stated she did not want to go back to surgery. In fact, she stated that she was willing to try anything to avoid further surgical intervention. The trauma care team had discussed taking the patient back to the OR the next day and possibly again later in the week for debridement and V.A.C.® Therapy dressing changes. However, I suggested to the trauma care team that V.A.C. VERAFLO™ Therapy using the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing could be used after a bedside debridement and performed by myself, in an effort to keep the patient out of the OR.I began preparation for placement of V.A.C VERAFLO™ Therapy following debridement. The patient was pre-medicated with IV morphine as available. The debridement started on the surgical wound that was located on the medial thigh. I performed a skin/subcutaneous tissue/muscle/fascia level surgical debridement with a total area debrided of 213.4 cm2. A minimal amount of bleeding was controlled with silver nitrate, and the procedure was well tolerated with a pain level of 0 throughout and a pain level of 0 following the procedure. Post debridement, the wound measured 22cm x 9.7cm x 6.1cm.
It was agreed that the bedside debridement and dressing use would be re-evaluated at minimum 2 days post therapy placement. There was significant improvement seen with respect to erythema, edema and wound volume after 3 days of V.A.C. VERAFLO™ Therapy with the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing. A second application of the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing was applied by a registered nurse on the wound care team with direct communication from myself regarding settings (refer to Table 1 for therapy details). The trauma team had discussed re-evaluating the wound after the weekend to determine if further debridement in the OR was necessary. On Day 6 of therapy, the second V.A.C. VERAFLO CLEANSE CHOICE™ Dressing was removed to reveal further reduction in wound size, with almost complete resolution of erythema and periwound edema. At this time, it was determined that the patient could be discharged to rehabilitation. The patient was so excited that her leg was beginning to look like a leg again. Due to the nature of the patient being discharged, debridement at the bedside was repeated and application of V.A.C.®, Therapy was placed. The patient did well and was medicated by bedside nursing. After debridement at the bedside, a V.A.C.® GRANUFOAM™ Dressing was applied, so that V.A.C.®Therapy could be resumed at the receiving facility as the patient would be discharged that same day.
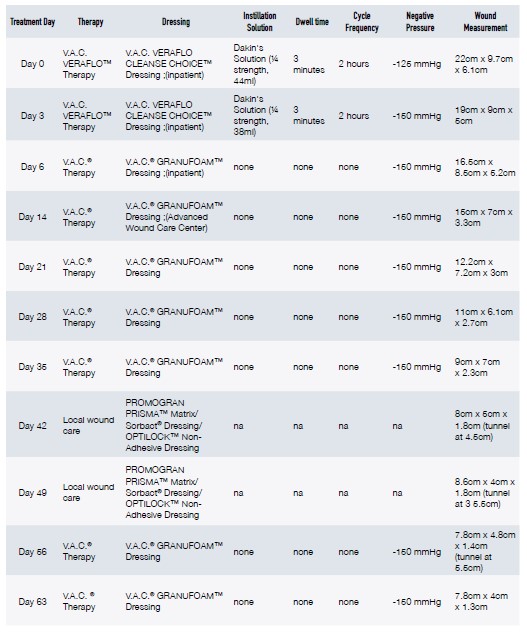
Since assuming care of the right medial thigh wound, and other healing wounds, we have made significant strides towards wound healing. The pattern in reduction of wound measurements can be seen in Table 1 along with photographic representations of the wound (Figures 1-6). Given the repeated failure to close the graft site and attempts to manage bacterial bioburden with standard V.A.C.® Therapy, I believe that V.A.C. VERAFLO™ Therapy using the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing was able to assist with healing of a stalled wound. There was marked reduction of edema/erythema and promotion of granulation tissue formation, such that optimal wound healing occurred. These benefits can be attributed to V.A.C. VERAFLO™ Therapy’s mechanisms of action: the cleansing during the instillation and dwell phase and the macrostrain and microstrain effects during the negative pressure phase.4-7 The success with this inpatient case has subsequently led to an increase in usage of V.A.C. VERAFLO™ Therapy with both the V.A.C. VERAFLO CLEANSE CHOICE™ Dressing and the standard V.A.C. VERAFLO™ Dressing at the Level 2 trauma center where I practice.
References
1.Agarwal A. Predictive Risk Factors for Incision Management. Chronicles of Incision Management: Clinical Insights, Perspective and Treatment Approaches. 2017;1:28-31.
2.Teot L, Boissiere F, Fluieraru S. Novel foam dressing using negative pressure wound therapy with instillation to remove thick exudate. Int Wound J. 2017;14:842-848
3.Gouin J-P, Kiecolt-Glaser JK. The Impact of Psychological Stress on Wound Healing: Methods and Mechanisms. Immunol Allergy Clin North Am. 2011;31:81-93.
4.Rycerz AM, Slack P, McNulty AK. Distribution assessment comparing continuous and periodic wound instillation in conjunction with negative pressure wound therapy using an agar-based model. Int Wound J. 2012;10:214-220.
5.Saxena SM, Hwang CW, Huang S, Eichbaum Q, Ingber D, Orgill P. Vacuum Assisted Closure: Microdeformations of Wounds and Cell Proliferation. Plast Reconstr Surg. 2004;114:1086-1096,1097-1098.
6.McNulty AK, Schmidt M, Feeley T, Kieswetter K. Effects of negative pressure wound therapy on the fibroblast viability, chemotactic signaling and proliferation in a provisional wound (fibrin) matrix. Wound Repair Regen. 2007;15:838-846.
7.McNulty AK, Schmidt M, Feeley T, Villanueva P, Kieswetter K. Effects of negative pressure wound therapy on cellular energetic in fibroblasts grown in a provisional wound (fibrin) matrix. Wound Repair Regen 2009; 17:192-199.