Dr. Allen Gabriel is a member of the American Society of Plastic Surgeons, and in 2001, Dr. Gabriel was chosen by the prestigious Loma Linda University to join the Integrated Plastic Surgery Residency Program. While at Loma Linda University, he volunteered on a medical mission to Ethiopia with Operation Good Samaritan. In addition, he served on several leadership committees and was the chief resident prior to completing his residency. In 2007, Dr. Gabriel was selected by world-renowned plastic surgeon Dr. G. Patrick Maxwell to enter a Breast and Aesthetic Surgery Fellowship in conjunction with Baptist Hospital in Nashville, Tennessee. Completion of this program provided him with advanced training in breast and aesthetic surgery.
Dr. Gabriel was one of the few medical students in the country to have received the prestigious Humanism in Medicine Award. This award lead to the creation of the University of Nevada’s Humanism in Medicine Honor Society, of which Dr. Gabriel is still an active member. During medical school, he was involved with both clinical and basic science research, earning several research awards and publications prior to graduating. Dr. Gabriel is board certified in plastic surgery and has been invited to speak nationally and internationally on breast and aesthetic surgery.
Gabriel_The Chronicles of Incision Management_2017_Volume 1_Issue 2
INTRODUCTION
Skin reducing mastectomies allow better shaping of the breast and long-term aesthetics, yet can result in complications post immediate breast reconstruction, particularly in obese (body mass index > 30kg/m2) patients and/or patients with large, pendulous breasts. The main limitations of the procedure are risks of seroma formation and ischemic necrosis of the thin flap, surgical site infection, and wound dehiscence. Positive clinical outcomes have been reported with use of closed incision negative pressure therapy (ciNPT; PREVENA™ Incision Management System) over various high-risk incision types, including arthroplasty, sternotomy, and cesarean.1-5 ciNPT provides a closed system that helps hold incision edges together, removes infectious materials, and protects the incision from external contamination.6 We have previously found that ciNPT is a viable option over incisions after immediate postmastectomy breast reconstruction.7 Here, we describe our initial experience with the use of ciNPT in a mastectomy patient whose incision area was predetermined to be low in perfusion post immediate breast reconstruction.
CASE STUDY
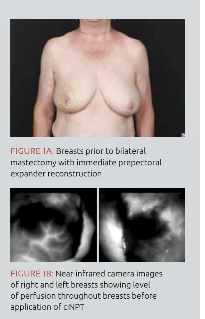
Patient was a 65-year-old female with a body mass index of 28 kg/m2 (Figure 1A). She underwent a bilateral skin sparing mastectomy with immediate expander reconstruction and received an acellular dermal matrix, which was used to reinforce the weakened skin flaps. The patient did not receive chemotherapy or radiation. Following completion of the mastectomy flap, the port expander was placed and dye was injected into the breast followed by measurement of tissue perfusion using a near-infrared camera to visualize blood flow and tissue perfusion (Figure 1B). Incision areas of concern for low perfusion were marked, and ciNPT was applied over the marked incision area for 7 days at -125mmHg (Figure 1C). The incision remained closed on postoperative Day 7 (Figure 1D), and there were no incidences of ischemic flap necrosis during use of ciNPT or follow-up. Three months after mastectomy and immediate reconstruction, the expanders were replaced with implants. The patient remained healed with no complications at 4 months after second stage implant exchange (Figure 1E).
CONCLUSIONS
Good aesthetic outcomes with no infection or implant loss were achieved in this patient with adjunctive use of ciNPT and well-planned operative procedures based on sound surgical principles. The thin flap incisions healed without complications over areas that were shown by near-infrared camera to have low perfusion immediately following breast reconstruction. In our experience, this technique allowed for optimal outcomes in a patient who previously may not have been considered for immediate prepectoral expander-implant breast reconstruction.
References
1.Pachowsky M, Gusinde J, Klein A et al. Negative pressure wound therapy to prevent seromas and treat surgical incisions after total hip arthroplasty. Int Orthop2012;36:719-722.
2.Grauhan O, Navasardyan A, Hofmann M, Muller P, Stein J, Hetzer R. Prevention of poststernotomy wound infections in obese patients by negative pressure wound therapy. J Thorac Cardiovasc Surg2013;145:1387-1392.
3.Grauhan O, Navasardyan A, Tutkun B et al. Effect of surgical incision management on wound infections in a poststernotomy patient population. Int Wound J2014;11:6-9.
4.Swift SH, Zimmerman MB, Hardy-Fairbanks AJ. Effect of single-use negative pressure wound therapy on postcesarean infections and wound complications for high-risk patients. J Reprod Med 2015;60:211-218.
5.Gunatilake RP, Swamy GK, Brancazio LR et al. Closed-Incision Negative-Pressure Therapy in Obese Patients Undergoing Cesarean Delivery: A Randomized Controlled Trial. American Journal of Perinatology Reports 2017;7:e151-e157.
6.Willy C, Agarwal A, Andersen CA et al. Closed incision negative pressure therapy: international multidisciplinary consensus recommendations. Int Wound J 2017;14:385-398.
7.Gabriel A, Sigalove SR, Maxwell GP. Initial Experience Using Closed Incision Negative Pressure Therapy after Immediate Postmastectomy Breast Reconstruction. Plastic and Reconstructive Surgery Global Open 2016;4:e819.