Dr. Fernandez is a Clinical Assistant Professor of Surgery and Family Practice at the University of Texas Health Center at Tyler. He is also an Attending Teaching Staff in the Division of Surgery for Mother Frances Health System and East Texas Medical Center in Tyler. Dr. Fernandez obtained his residency training at Loyola University, the University of Illinois, the University of Chicago and Northwestern University, Chicago, Illinois, with special training in Trauma and Burns at Kings County Hospital, SUNY Down State System, Brooklyn, New York, NY. He is well-published in multiple areas of research, both in peer-reviewed articles and book chapters, and has made numerous oral and poster presentations at national and international conferences.
Fernández_The Chronicles of Incision Management_2017_Volume 1_Issue 1
Epidemiology
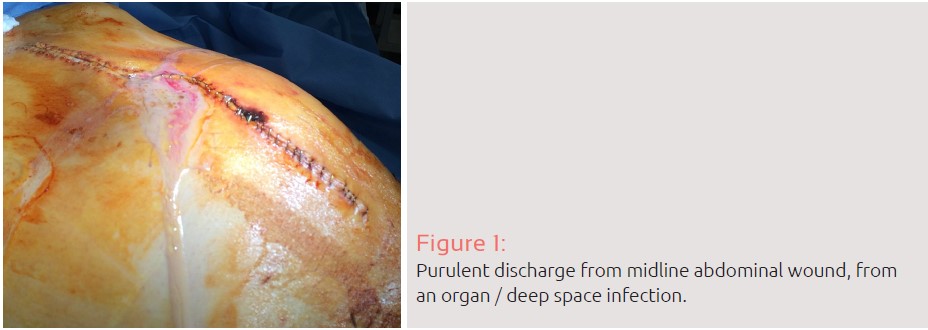
Infection at or near surgical incisions within 30 days of an operative procedure, known as surgical site infection, contributes substantially to surgical morbidity and mortality each year.
Surgical site infections (SSIs) occur frequently and are morbid and are now the most common and costly of all hospital-acquired infections, with a reported incidence ranging from 15-37%.1, 2, 4 Figure 1.
As reported by Ban, Kristen A. et al., surgical site infections are associated with increased length of stay and a 2- to 11-fold increase in the risk of mortality.
Although most patients recover from an SSI without long-term adverse sequelae, 77% of mortality in patients with an SSI can be attributed to the infection itself.
The high incidence of surgical site infections in abdominal trauma requires knowledge of the management of the traumatic injury itself but also all of the complications associated with it. Surgical infections are frequent complications in this patient population, with an incidence of intra-abdominal infections/abscess that ranges between 2% and 12%.
Definitions
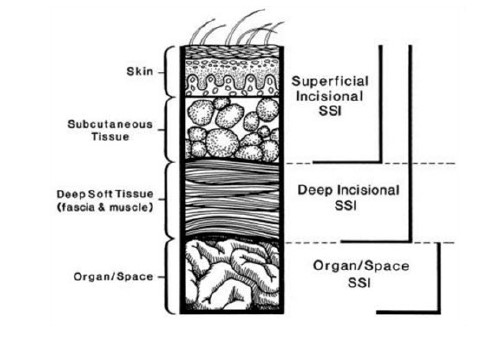
The most widely used definition of SSI has been provided by Centers for Disease Control and Prevention (CDC). According to this definition, SSIs are classified by depth and tissue spaces involved.
There are 3 different types of surgical site infections. In the criteria put forth by the CDC, SSIs are either incisional or organ/space, with incisional SSIs being further sub classified as superficial (involving only skin and subcutaneous tissue) versus deep (involving underlying soft tissue).
Cost
Surgical site infections raise costs due to prolonged hospitalization, additional diagnostic tests, prolonged use of antibiotic treatment, and re-operative surgical interventions.13 In the most recent (2009) report, the presence of SSI increased the length of stay in the intensive care unit, as well as total hospital stay (the latter by 9-10 days). This increased costs of care by $20,842 per patient admission, with additional hospital costs exceeding $900 million. For surgical infections requiring hospital readmission, an additional cost of $700 million in health care spending was noted.
Intra-abdominal infections raise costs more than superficial infections.15 A study examining the cost of SSIs revealed an increase of 115% for the cost of care of patients with an SSI as compared to without surgical site infections.
Microbiology
In the majority of infections, the pathogen comes from the native flora of the patient’s skin, mucous membranes, or hollow viscera.17 Skin infections are more commonly caused by aerobic gram-positive cocci such as Staphylococcus, with resistant organisms, such as methicillin-resistant S aureus (MRSA), representing a growing segment of these infections.18, 19 Figure 4, 5
In contaminated cases that require or present with an opening in a hollow viscus, gram-negative bacilli such as Escherichia coli, gram-positive organisms such as enterococcus, anaerobic organisms such as Bacillus fragilis, and, rarely, yeast and viral pathogens are found.11, 20 Figure 6
The Trauma/ Acute Care Surgical Patient
Morales, Escobar, et al. conducted a prospective cohort study between November 2000 and March 2002 involving 614 patients who underwent emergent exploratory laparotomy. In their report, they noted
that trauma patients undergoing emergent surgery had a high incidence of infection, up to 37%. Nosocomial infection was the source in 75% of all SSI, with 22% attributed to the initial injury. Only 2% of patients in their study had infections present at the time of initial surgical intervention. Trauma/Acute Care Surgical patients have a high rate of organ/intra-abdominal SSIs (12%).
Risk Factors
Commonly reported risk factors such as advanced age, type of trauma, the presence of shock, high ISS scores, prolonged mechanical ventilation, multiple transfusions, and multiple surgical procedures (among others) have been reported to contribute to infections in trauma patients.
Morales et al. found that the independent variables statistically associated with SSI complications were an Abdominal Trauma Index score greater than 24, abdominal contamination and admission to the intensive care unit.
Duration of operation
A similar recent study found that the SSI rate in patients with duration of operation < 3 hours was 20.9% and 50% in those which had duration of operation ≥ 3 hours, with a statistically significant association between the duration of operation and SSI (p-value = 0.0001).
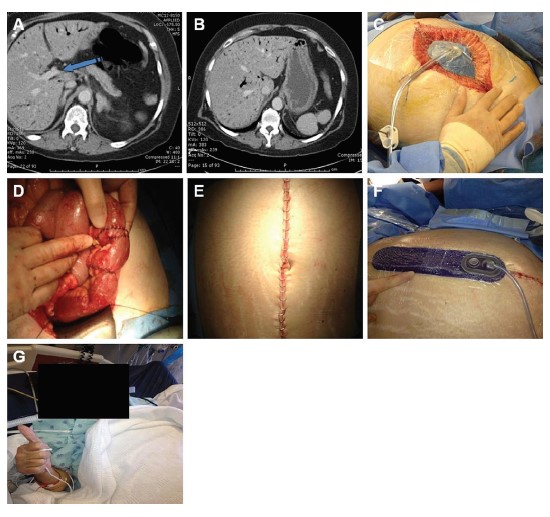
Results of the Use of Negative Pressure Therapy in the Management of Surgical Incisions
Cantero, et al. conducted a recent prospective interventional pilot study at La Paz University Hospital, a tertiary care academic center in Madrid, Spain. The PREVENA™ Incision Management System was applied on the wounds of 17 consecutive patients undergoing ileostomy reversal. Forty-three patients undergoing the same procedure were treated with conventional dressings served as the control group.
The primary end point of the study was the detection of SSI utilizing the Centers for Disease Control definition criteria. All procedure-related complications were noted as well. They found no significant differences in demographic variables between groups. In the control group, 9 patients (21%) presented SSI, with statistical significance (P < .038) when compared with the intervention group (0%). There were no complications associated with the application of the PREVENA™ Therapy. Other complications not related to the use of negative pressure therapy (e.g., ileus or obstruction) occurred in 30% of patients. The authors concluded that the negative-pressure PREVENA™ Incision Management System was safe and easy to use and may have an effect on SSIs in dirty-contaminated wounds such as those from ileostomy closure.
This author’s similar experience with the use of negative pressure therapy in this patient population was recently reported, with a similar conclusion.28Figure 7
In a similar report of use of incisional negative pressure at -75 mmHg Bonds, et al. looked at all patients undergoing open colectomy at a single institution tertiary academic medical center, from 2009 through 2011. The primary outcome measured was the presence or absence of surgical site infection. Of the 254 patients in this study, 69 (27.2%) developed a surgical site infection; 4 (12.5%) surgical site infections were seen in patients undergoing incisional negative pressure wound therapy and 65 (29.3%) were seen in patients undergoing standard closure. In their analysis of the data the authors found that diabetes mellitus increased the chance of surgical site infection (OR, 1.98; p < 0.05), and that the use of incisional negative pressure wound therapy decreased the chance of surgical site infection (OR, 0.32; p < 0.05). They also noted that obesity was associated with a trend toward increasing surgical site infection as well (OR, 1.64; p = 0.10). The authors concluded that incisional negative pressure wound therapy appears to reduce surgical site infection in open colorectal surgery.
Conclusions
Although further study is needed to further define the optimal patient populations for the use of this technique, these and other recently published reports appear to suggest that NPWT is safe, easy to use, and may be applied to incisions over potentially contaminated wounds, not frankly contaminated or ischemic wounds, in varied surgical settings with the expectation of impact on post-surgical outcomes.
Resources and Further Reading for the Trauma Acute Care Surgeon
Surgical site infections are a major problem in the modern Trauma / Acute Care surgical wards. Methods aimed at prevention of infection in the operating room have varying levels of data to substantiate their practice. Various organizations have developed guidelines for the prevention of SSI. The differences that exist in these recommendations are due to the absence of high-quality data as well as the variable interpretation of existing data although imperfect; these guidelines create the framework for delivery of evidence-based care.
Sample Guidelines
•WHO Global guidelines on the prevention of surgical site infection
•http://www.who.int/gpsc/ssi-guidelines/en/
•CDC and HICPAC DRAFT Guideline for Prevention of Surgical Site Infection
•http://c.ymcdn.com/sites/www.cste.org/resource/dynamic/forums/20130319_111419_13595.pdf
•American College of Surgeons and Surgical Infection Society: Surgical Site Infection Guidelines, 2016 Update. Journal of the American College of Surgeons.
•Doi: http://dx.doi.org/10.1016/j.jamcollsurg.2016.10.029.
•Surgical site infection: prevention and treatment of surgical site infection.
•National Collaborating Centre for Women’s and Children’s Health. Surgical site infection: prevention and treatment of surgical site infection. London (UK): National Institute for Health and Clinical Excellence (NICE); 2008 Oct. 142 p. (Clinical guideline; no. 74). [256 references]
•Doi: https://www.guideline.gov/summaries/summary/13416/surgical-site-infection-prevention-and-treatment-of-surgical-site-infection?q=SSI
References
1.Risk factors associated with surgical site infection in upper and lower gastrointestinal surgery. Watanabe A, Kohnoe S, Shimabukuro R, Yamanaka T, Iso Y, Baba H, Higashi H, Orita H, Emi Y, Takahashi I, Korenaga D, Maehara Y. Surg Today. 2008;38(5):404–12.
2.Anderson, D.J., Podgorny, K., Berrios-Torres, S.I. et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35:605–627.
3.Ban, Kristen A. et al. American College of Surgeons and Surgical Infection Society: Surgical Site Infection Guidelines, Journal of the American College of Surgeons 2016 Update. 224;1:59–74.
4.Magill, S.S., Edwards, J.R., Bamberg, W. et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370:1198–1208.
5.Smyth ET. Surgical site infection surveillance. J Hosp Infect. 2000;45:173–84. [PubMed]
6.Berard F, Gandon J. Postoperative wound infections: the influence of ultraviolet irradiation of the operating room and of various other factors. Ann Surg. 1964;160(Suppl 2):1–192. [PubMed]
7.Weigelt JA, Haley RW, Seibert B. Factors influence the risk of wound infection in trauma patients. J Trauma. 1987;27:774–81. [PubMed]
8.National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 to June 2004, issued October 2004. [accessed 2009 Aug. 1]. Available: www.cdc.gov/ncidod/hip/NNIS/2004NNISReport_AJIC.PDF.
9.Morales CH, Villegas MI, Villavicencio R, et al. Intra-abdominal infection in patients with abdominal trauma. Arch Surg. 2004;139:1278–85. [PubMed]
10.Deitch EA, Livingston DH, Hauser CJ. Septic complications in the trauma patient. New Horizons. 1999;7:158–72.
11.Mangram AJ, Horan TC, Pearson ML, et al. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97–132. Quiz 133–134; Discussion 96.
12.Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13(10):606–8.
13.Urban JA. Cost analysis of surgical site infections. Surg Infect (Larchmt) 2006;7(suppl 1):S19–S22. [PubMed]
14.de Lissovoy G, Fraeman K, Hutchins V, et al. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009;37:387–397. [PubMed]
15.Vegas AA, Jodra VM, Garcia ML. Nosocomial infection in surgery wards: a controlled study of increased duration of hospital stays and direct cost of hospitalization. Eur J Epidemiol. 1993;9:504–510. [PubMed]
16.Broex EC, van Asselt AD, Bruggeman CA, van Tiel FH. Surgical site infections: how high are the costs? J Hosp Infect. 2009;72:193–201. [PubMed]
17.Altemeier WA, Culbertson WR, Hummel RP. Surgical considerations of endogenous infections- sources, types, and methods of control. Surg Clin North Am. 1968;48:227–240. [PubMed]
18.Schaberg DR. Resistant gram-positive organisms. Ann Emerg Med. 1994;24:462–464. [PubMed]
19.Schaberg DR, Culver DH, Gaynes RP. Major trends in the microbial etiology of nosocomial infection. Am J Med. 1991;91(3B):72S–75S. [PubMed]
20.Giamarellou H, Antoniadou A. Epidemiology, diagnosis, and therapy of fungal infections in surgery. Infect Control Hosp Epidemiol. 1996;17:558–564. [PubMed]
21.Morales CH, Escobar RM, Villegas MI, Castaño A, Trujillo J. Surgical site infection in abdominal trauma patients: risk prediction and performance of the NNIS and SENIC indexes. Canadian Journal of Surgery. 2011;54(1):17–24. Doi: 10.1503/cjs.022109.
22.Papia G, McLellan BA, El-Helou P, et al. Infection in hospitalized trauma patients: incidence, risk factors, and complications. J Trauma. 1999;47:923–33. [PubMed]
23.Caplan ES, Hoyt NJ. Identification and treatment of infections in multiply traumatized patients. Am J Med. 1985;79(Suppl 1A):68–76. [PubMed]
24.Weigelt JA, Haley RW, Seibert B. Factors which influence the risk of wound infection in trauma patients. J Trauma. 1987;27:774–81. [PubMed]
25.Baker JW, Deitch EA, Li M, et al. Hemorrhagic shock induces bacterial translocation from the gut. J Trauma. 1988;28:896–906. [PubMed]
26.Mawalla B, Mshana SE, Chalya PL, Imirzalioglu C, Mahalu W. Predictors of surgical site infections among patients undergoing major surgery at Bugando Medical Centre in Northwestern Tanzania. BMC Surgery. 2011;11:21. Doi:10.1186/1471-2482-11-21.
27.Cantero, Ramon MD, PhD; Rubio-Perez, Ines MD, PhD; Leon, Miguel MD; Alvarez, Mario MD; Diaz, Beatriz MD; Herrera, Ana MD; Diaz-Dominguez, Joaquin MD, PhD; Rodriguez-Montes, Jose Antonio MD, PhD. Negative-Pressure Therapy to Reduce the Risk of Wound Infection Following Diverting Loop Ileostomy Reversal: An Initial Study. Advances in Skin & Wound Care: 2016;29(3):114–118. Doi: 10.1097/01.ASW.0000480458.60005.34
28.Fernández LG, Management of the open abdomen: clinical recommendations for the trauma/acute care surgeon and general surgeon. Int Wound J. 2016 Sep;13 Suppl 3:25–34. Doi: 10.1111/iwj.12655.
29.Bonds AM, Novick TK, Dietert JB, Araghizadeh FY, Olson CH (2013) Incisional negative pressure wound therapy significantly reduces surgical site infection in open colorectal surgery. Dis Colon Rectum 56(12):1403–1408. [PubMed]
30.Semsarzadeh NN, Tadisina KK, Maddox J, et al. Closed incision negative-pressure therapy is associated with decreased surgical-site infections. Plast Reconstr Surg 2015; 136:592–602. [PubMed]
31.Stannard JP, Robinson JT, Anderson ER, et al. Negative pressure wound therapy to treat hematomas and surgical incisions following high-energy trauma. J Trauma 2006; 60:1301–1306. [PubMed]
32.Moues CM, Heule F, Hovius SER. A review of topical negative pressure therapy in wound healing: Sufficient evidence? Am J Surg 2011; 201:544–556. [PubMed]
33.Mark KS, Alger L, Terplan M. Incisional negative pressure therapy to prevent wound complications following cesarean section in morbidly obese women: a pilot study. Surg Innov 2014; 21:345–349. [PubMed]
34.Grauhan O, Navasardyan A, Hofmann M, et al. Prevention of poststernotomy wound infections in obese patients by negative pressure wound therapy. J Thorac Cardiovasc Surg 2013; 145:1387–1392. [PubMed]