Literature Synopsis_The Chronicles of Incision Management_2017_Volume 1_Issue 2
INTRODUCTION
In the U.S., close to a third of all babies are born via Caesarean delivery,1making this procedure the most common surgery in the country. About 2-7% of such deliveries result in surgical site occurrences (SSOs) that raise the risk of infection, complicate recovery, and incur extra costs.2,3 Maternal obesity (BMI > 30) is a key risk factor for post-Caesarean wound morbidity.
Evidence from previous studies suggests that closed incision negative pressure therapy (ciNPT) may decrease the rate of postoperative infection and wound dehiscence.6 This study sought to compare clinical outcomes in obese women who received ciNPT or standard-of-care (SOC) dressings following Caesarean delivery.
METHODS
Study design
This single-center post-marketing RCT enrolled 92 patients from Duke University Medical Center between 2012 and 2014. Subjects were ≥ 18 years old and had a BMI of ≥ 35 at the time of delivery. Women with skin, systemic, or chorioamniotic infections and those at high risk for anesthesia were excluded from participation.
Protocol
Participating clinicians used standard techniques to prepare subjects for the operation, perform it, and close the wounds. All women received preoperative antibiotics and post-operative pain medications as required (not standardized in the protocol). The peritoneum was left open and the adipose tissue was sutured if thicker than 2 cm. Once the closed wounds passed inspection, patients were randomized 1:1 to ciNPT and SOC groups.
Women in the ciNPT group received a sterile “peel-and-place” multilayer dressing over the closed incision. The dressing’s tubing was then connected to a negative pressure unit that delivered -125 mmHg of continuous pressure to the dressing for 5 to 7 days and removed exudates. Women in the SOC group had their wounds dressed with Steri-Strips (Trademark of 3M Health Care, St. Paul, MN) sterile gauze, and Tegaderm (Trademark of 3M Health Care, St. Paul, MN) for 1-2 days. Subjects without complications were discharged from hospital 3-4 days postoperatively.
Endpoints
The primary endpoint was the presence of one or more postoperative SSOs (counted as one event per affected patient, regardless of the number of SSOs in that patient). These SSOs included inflammatory responses, prolonged drainage, fluid collection, dehiscence, and surgical site infections. A standardized wound-scoring system minimized bias. The secondary endpoint was the use of surgical interventions such as antimicrobials, surgical drainage, incision packing, adjunctive negative pressure therapy, debridement, and reoperation. Supplementary endpoints included postoperative pain scores ≥ 2 (Baker Faces Scale) at rest and with pressure. Medication use was also recorded.
Patient characteristics
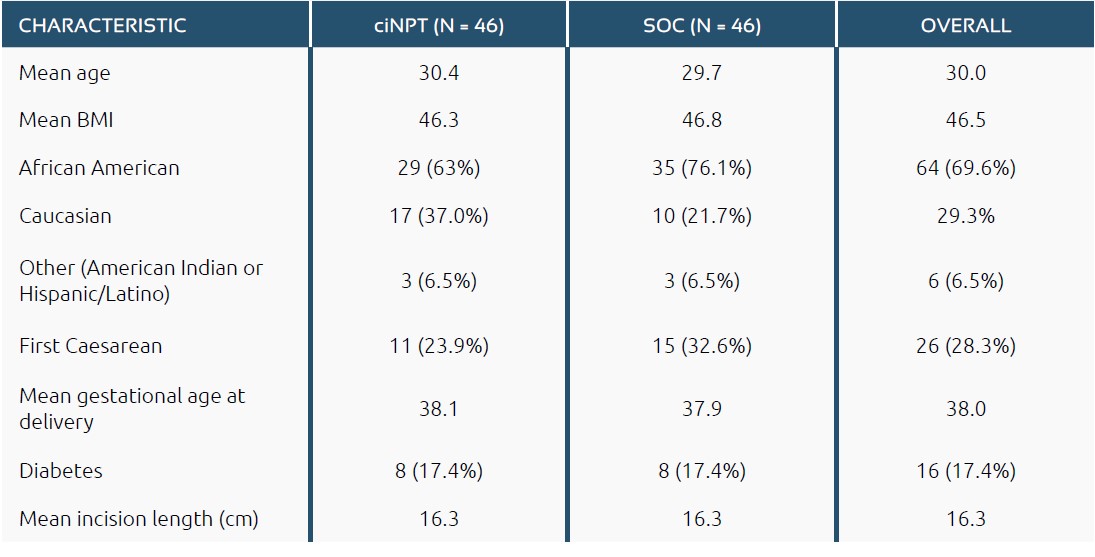
Collected data included age, BMI, gestational age at delivery, and first vs repeat Caesarean section (Table 1). The study population included ethnic groups described as African American, Caucasian, American Indian and Hispanic/Latino. Other than the higher proportion of African American subjects in the SOC group than the ciNPT group, patient characteristics were similar in the two groups.
RESULTS
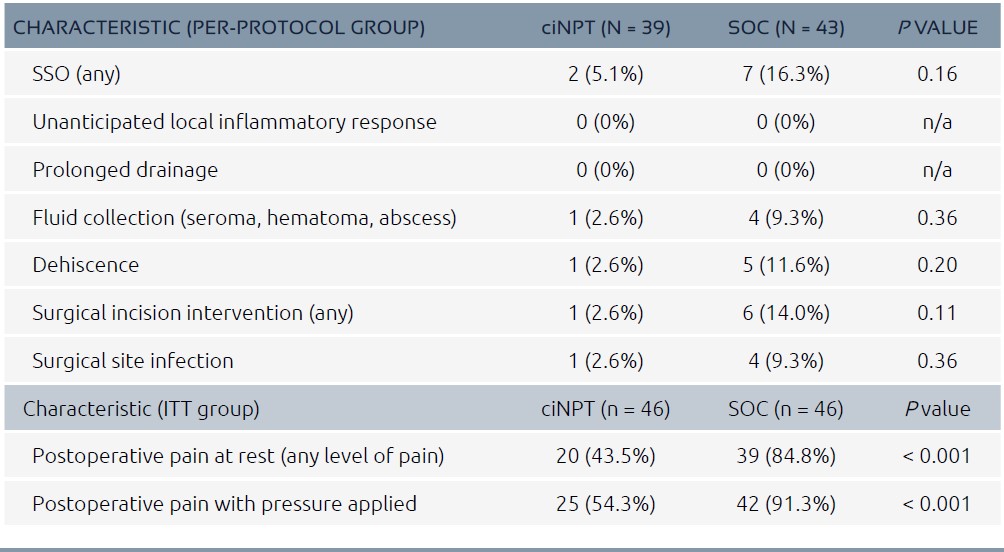
Pain results are reported for the intention-to-treat (ITT) population (n = 96); all other results pertain to the per-protocol population (n = 92). Per-protocol results were analyzed using SAS version 9.2. As detailed in Table 2, the ciNPT group had a 63% relative reduction in patients with SSOs compared to the SOC group, though the difference did not reach statistical significance. In terms of specific SSOs, the ciNPT group had:
•Fewer cases of fluid collection (1 vs 4, p = 0.36)
•Fewer cases of dehiscence (1 vs 5, p = 0.20)
•Fewer cases of surgical incision intervention (1 vs 6, p = 0.11)
The ciNPT group had a significantly lower rate of postoperative pain at rest (43.5 vs. 84.8%, p < 0.001) and with pressure (54.3 vs 91.3%, p < 0.001). Total narcotic use was 30% lower in the ciNPT group than the SOC group (p = 0.036), while acetaminophen and NSAID use did not differ significantly between the groups.
DISCUSSION
This study demonstrated that, compared to the standard of care for women undergoing Caesarean deliveries, ciNPT is associated with a significant reduction in postoperative pain and with a trend toward reduced wound complications.
The reduction in incisional pain in the ciNPT group, corroborated by a lower use of narcotic medications, has significant implications, given that ineffective pain relief may affect breastfeeding and bonding as well as increasing the risk of thromboembolism.7,8While not statistically significant, the reduction in SSOs with ciNPT is also clinically relevant due to the substantial morbidity and costs of surgical site infections (a component of the primary outcome).
Previous investigations of post-Caesarean ciNPT have yielded mixed results. One case-control study found no reduction in surgical site infections with ciNPT compared to historical controls.9 In contrast, a prospective case-control study found a significant 70% reduction in wound complications with ciNPT versus historical controls,10 and a study of obese women yielded no postoperative complications in the ci-NPT-treated group (vs 10% in the control group).
This study adds to the body of evidence regarding ciNPT following Caesarean delivery. There is a need for further, more strongly powered studies to examine the impact of ciNPT in risk-diverse obstetric populations.
References
1.Centers for Disease Control and Prevention. Births—Method of delivery. Available at: http://www.cdc.gov/nchs/fastats/delivery.htm
2.Edwards J R, Peterson K D, Mu Y et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control 2009;37:783–805.
3.Perlow J H, Morgan M A, Montgomery D et al. Perinatal outcome in pregnancy complicated by massive obesity. Am J Obstet Gynecol 1992;167:958–962.
4.Alanis MC, Villers MS, Law TL et al. Complications of cesarean delivery in the massively obese parturient.Am J Obstet Gynecol 2010;203:2710–2712.
5.Olsen MA, Butler AM, Willers DM et al. Risk factorsfor surgical site infection after low transversecesarean section.Infect Control Hosp Epidemiol 2008;2906:477–484.
6.Stannard JP, Volgas DA, McGwin G et al. Incisional negative pressure wound therapy after high-risk lower extremity fractures. J Orthop Trauma 2012;26:37–42.
7.Gadsden J, Hart S, Santos AC. Post-cesarean delivery analgesia. Anesth Analg 2005;101(5 Suppl):S62–S69.
8.Woods AB, Crist B, Kowalewski S et al. A cross-sectional analysis of the effect of patient-controlled epidural analgesia versus patient controlled analgesia on postcesarean pain and breastfeeding. J Obstet GynecolNeonatal Nurs 2012;41:339–346.
9.Gibbs C, Orth T, Gerkovich M et al. Traditional dressing compared with an external negative pressure system in preventing wound complications. Obstet Gynecol2014;123:145S.
10.Swift SH, Zimmerman MB, Hardy-Fairbanks AJ. Effect of single-use negative pressure wound therapy on postcesarean infections and wound complications for high-risk patients. J Reprod Med 2015;60:211–218.
11.Mark KS, Alger L, Terplan M. Incisional negative pressure therapy to prevent wound complications following cesarean section in morbidly obese women: a pilot study. Surg Innov 2014;21:345–349.