
Dr. Laura Swoboda is a translational scientist, family nurse practitioner, and practicing wound specialist in Milwaukee, Wisconsin. In addition to providing direct patient care, Dr Swoboda serves as principal investigator for quality improvement, evidence-based practice, and research projects in complex wound care. They serve on the board of directors for the WOCNCB and the AAWC, on the NPIAP’s prophylactic dressing standards initiative task force, and the American Heart Association’s Peripheral Arterial Disease National Action Plan. Laura Swoboda is a paid consultant of Solventum.
Swoboda_Current-Dialogues-in-Wound-Management_2024_Article-1
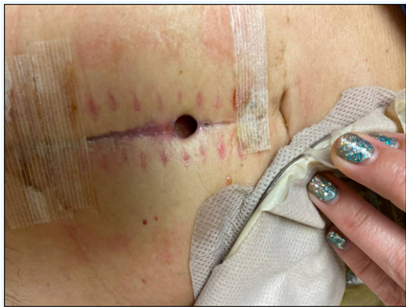
CASE REPORT: A 47-year-old female with a medical history of perforated sigmoid viscus underwent an exploratory laparotomy, which resulted in bowel resection and anastomosis. Unfortunately, the patient developed abscesses with left sided peritonitis and returned to the operating room for an anastomotic leak. During this second surgery, the patient had another exploratory laparotomy, resection of the sigmoid anastomosis, and the formation of a diverting end colostomy. The patient was discharged to home with a three-day course of cefdinir, metronidazole, and fluconazole. Approximately 1 week after discharge, the surgical incision dehisced. The patient then sought care at a hospital-based outpatient wound center in Southeastern Wisconsin for the abdominal wound. Prior to presentation the patient had been treated with iodine gauze. Upon arrival at the wound center the wound dimensions were 0.9 cm x 0.7 cm x 1.4 cm with circumferential undermining. Significant undermining was noted beneath the epithelialized portion of the surgical incision (Figure 1), with the deepest portion of undermining measuring 6 cm at the 6 o’clock position. The small opening limited direct visualization of the wound base, thorough cleansing of the wound, and application of advanced therapies to the wound base. A 3M™ Promogran Prisma™ Collagen Matrix with ORC and Silver dressing was applied, and the wound was covered with a silicone-bordered adhesive foam dressing until the patient could return the following day for a surgical sharp debridement and negative pressure wound therapy. The following day, the wound was surgically debrided along the epithelialized portion of the incision in both caudal and pedal directions to the extent of the undermining (Figure 2).
The wound treatment plan was adjusted to address and prevent common barriers to healing. The wound and peri-wound were cleansed with mild soap and water. Hypochlorous acid was applied to the wound and periwound tissues and allowed to soak (ensuring a consistent wet surface where applied) for a minimum of 3 minutes per treatment. The periwound skin was protected with a no-sting barrier wipe. During visits with the wound specialist, the patient underwent sharp debridement to remove necrotic tissue and bioburden, address biofilm, refashion the wound edges to allow for centripetal epithelium migration, and expose the endothelium of blood vessels to reinitiate the healing cascade. The patient then began a combination of Promogran Prisma Matrix, fenestrated by hand, applied to the wound bed along with 3M™ ActiV.A.C.™ Therapy System. The periwound was further protected by window framing the wound with a transparent drape as needed. Promogran Prisma Matrix was applied in a single layer to the wound base including undermining. 3M™ V.A.C.® Granufoam™ Dressing was placed over the wound and was covered with a transparent drape. The negative pressure wound therapy was set to -125 mmHg. The wound was assessed and treated 3 times per week (every 48-72 hours), with the cannister being changed weekly or as needed.
At the 2-week follow-up, (Figure 3), the wound showed reduced undermining and depth with increased granulation across the exposed abdominal fascia. The combined use of Promogran Prisma Matrix and the ActiV.A.C. Therapy System was continued for an additional 2 weeks. At the subsequent follow-up, the wound was flush, and granulation tissue covered the wound base (Figure 4). Promogran Prisma Matrix and the ActiV.A.C. Therapy System use was discontinued. The patient was transitioned to a silicone-bordered super absorbent polymer dressing, which was changed weekly until the wound epithelialized 2 weeks later (Figure 5).




DISCUSSION: This case illustrates the combined use of Promogran Prisma Matrix and ActiV.A.C. Therapy System over a 4-week period to manage a complex dehisced abdominal incision with circumferential undermining following multiple surgical revisions. After 40 days, the wound was completely epithelialized. In this patient, the strategy of combined use of Promogran Prisma Matrix and the ActiV.A.C. Therapy System was effective for wound management. Bacteria and pro-inflammatory factors can prolong the inflammatory phase and preempt wound healing. The Promogran Prisma Matrix can optimize the moist wound environment for healing,1,2 while the ActiV.A.C. Therapy System provides a closed, moist wound healing environment and promotes granulation tissue development.3,4 This case exemplifies the positive outcomes achieved through the use of wound bed preparation and best practices in the real-world challenges of wound management. To minimize wound healing impairment, providers must be cognizant of potential wound healing complications and plan for mitigation strategies. The Promogran Prisma Matrix was chosen for its ability to promote a moist wound environment which is conducive to the development of granulation tissue, re-epithelialization, and optimal wound healing. Negative pressure wound therapy offers complementary benefits, including supporting wound edges, providing microstrain, removing inflammatory exudates, stimulating granulation tissue, and protecting wound tissues. In this case of a complex dehisced abdominal incision, the combined use of Promogran Prisma matrix and ActiV.A.C. Therapy System was both effective and safe.
SUMMARY: This case highlights the successful combined use of Promogran Prisma Matrix and the ActiV.A.C. Therapy System to achieve durable wound healing. This approach provides healthcare providers with versatile tools to address complex wound management, ultimately benefiting patients.
References
- Gottrup F, Cullen BM, Karlsmark T, Bischoff-Mikkelsen M, Nisbet L, Gibson MC. Randomized controlled trial on collagen/oxidized regenerated cellulose/ silver treatment. Wound Repair Regen. 2013;21(2):216-225. doi:10.1111/ wrr.12020
- Shu H, Xia Z, Qin X, et al. The clinical efficacy of collagen dressing on chronic wounds: A meta-analysis of 11 randomized controlled trials. Front Surg. 2022;9:978407. doi:10.3389/fsurg.2022.978407
- Saxena V, Hwang CW, Huang S, Eichbaum Q, Ingber D, Orgill DP. Vacuum-assisted closure: microdeformations of wounds and cell proliferation. Plast Reconstr Surg. 2004;114(5):1086-1096. doi:10.1097/01. prs.0000135330.51408.97
- McNulty AK, Schmidt M, Feeley T, Kieswetter K. Effects of negative pressure wound therapy on fibroblast viability, chemotactic signaling, and proliferation in a provisional wound (fibrin) matrix. Wound Repair Regen. 2007;15(6):838- 846.
NOTE: Specific indications, contraindications, warnings, precautions and safety information exist for these products and therapies. Please consult a clinician and product instructions for use prior to application. Rx only.
As with any case study, the results should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Patient data and images courtesy of Laura Swoboda, DNP, APNP, FNP-BC, CWOCN-AP.
© Solventum 2024.

