Ms. Patricia Hotaling is a registered nurse, who is board certified in gerontological gursing. She was a unit manager and a wound care nurse of a long-term care and skilled nursing facility for 18 months, an acute care nurse for over 5 years, and has a passion for hospice and palliative care. Ms. Hotaling currently teaches undergraduate baccalaureate students for the University of Nebraska Medical Center, where she will graduate with her doctorate of nursing practice in December 2018.
Hotaling_Current Dialogues in Wound Management_2018_Volume 4_Issue 4
Today’s healthcare environment is highly focused on clinical outcomes and the regulations to achieve them. For example, issues such as skin integrity, pain management, falls, and medication errors are closely monitored to evaluate the quality and safety of the care provided. Additionally, pressure injuries (PIs) are one of the many benchmarking measures used to appraise quality nursing care. However, unlike the falls and medication errors that happen quickly, PIs take hours to form, and the open wound lasts for weeks to months. The director of nurses (DON) has many responsibilities in the prevention and management of PIs.
ROLES AND RESPONSIBILITIES
Assessment of the wounds and PIs is an important task the DON delegates. The wound care team is a delegate branch of the DON that is trained to assess the wound, analyze the wound progress (or lack thereof), determine a correct treatment plan, perform complex dressing changes, and train staff nurses to complete less complex dressing changes. This group must have the correct training and tools to complete this role, as well as a consistent plan for completing standards of practice such as weekly measurements, and communicating with providers and the larger care team. While a licensed practical nurse or a licensed vocational nurse can measure a wound, the DON must ensure a registered nurse is correctly and consistently performing a PI assessment with staging upon discovery of the wound and, at least weekly, to align with scope and standards of practice.
Given the director’s responsibility of providing current and appropriate care, the DON must stay up to date in wound therapy. The nearly continuous changes in wound care can make it seem impossible for a non-wound care provider to stay current (J. Black, written communication, September 2018). Sometimes, the difficulty lies in needing to affirm the correct treatments are being done for patients, but the DON may not know the current evidence. The wound care team should be expected to bring back knowledge obtained from continuing education opportunities and provide a synopsis to the director and their teammates about new and advancing science in wound care. While medical supply companies that provide wound care products often have trained salespersons, it is not best practice to be educated solely by industry (J. Black, written communication, September 2018).
CREATING SYSTEMS TO FACILITATE COMMUNICATION
The DON is also responsible for having proper systems in place to provide care to the patients, as well as utilizing resources appropriately. To do this, the director needs to work closely with the in-house wound care team to ensure providers are being communicated with appropriately. For example, if the provider is informed of the development of a stage 2 PI, the provider must be told when it deteriorates into a larger or deeper wound. This communication is designed to avoid the provider incorrectly repeatedly documenting “stage 2” when the ulcer has evolved. When this happens, it would appear that the staff was not communicating about the true condition of the PI.
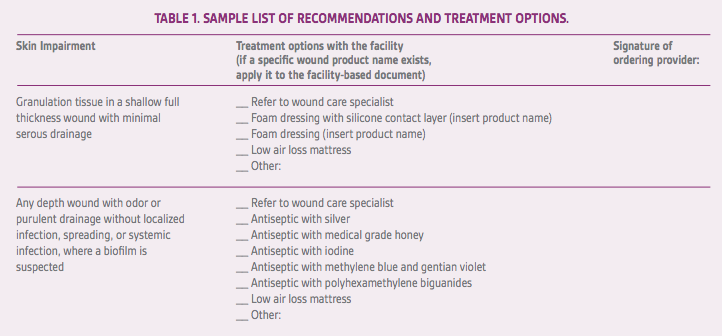
The wound care team is strongly encouraged to prepare and provide a list of evidence-based recommendations, including available treatments, for different wounds (see Table 1). It is also vital that the DON and/or administrator maintain a contract with a manufacturer of wound care products to ensure enough variety of dressings is available to treat different wounds. The director should plan ahead to provide additional resources for patients who are at high risk of developing PIs, such as upscaled beds and prophylactic dressings. These interventions can be discussed with the wound care team to ensure the proper interventions are being used.
Monitoring compliance with turning schedules may seem out of the expectations for the director, and while the DON may not see patients often, a plan must be in place to ensure that patient turning is completed on time and as required. There are 2 vital components to turning: frequency and adequacy. In my experience, the frequency is commonly accepted as being every 2 hours; however, that schedule is modifiable. A reasonable approach is to turn all the residents toward the window at the same time, then onto their backs for meals and toward the door on the next turn. This method allows visualization of compliance without having to enter each room. Adequacy of the turn means that a 30-degree lateral angle is achieved and is best measured by checking to see if the sacrum is off the bed when the resident is turned.
OVERSIGHT OF WOUND CARE
Both the director and wound care team are responsible for ensuring that the staff understands:
1)How to change dressings using clean technique.
2)The frequency of dressing changes.
3)Where to document completion.
4)How to document findings that indicate wound deterioration.
5)Who to notify with questions or concerns about the wound.
Pressure injuries require skilled nursing care to perform dressing changes, regardless of how frequent the changes occur. These wounds also require registered nurses to assess, measure, and stage them on a weekly basis. Skilled nursing facilities can use these nursing interventions to maintain a resident on skilled services on Medicare part A.
Large companies owning multiple facilities have been a model of business for a long time. The parent company must ensure proper nursing care is being provided at each facility. To ensure monitoring is accurate, a list of all PIs is often maintained. These can be reported weekly as the number of stage 1s, stage 2s, stage 3s, and so on. It is imperative that only PIs be reported and that the PI is staged correctly. Accuracy of diagnosis and staging must be determined by the wound team. If patient behaviors are interfering with wound care, an interdisciplinary team (IDT) meeting with the patient to show the potential complications may help reduce or eliminate the behaviors.
UTILIZING THE IDT
A significant change in condition occurs when the PI or another wound first appears and again if it worsens. A resolved wound is not a “significant change,” however a change in the plan of care is needed. An IDT care meeting should include a dietitian, social services, therapeutic recreation, nursing, and any other discipline that needs to be involved. In addition, the meeting should encompass the changes that need to be made to the plan of care based on the current condition. Dietitians can review for adequate calories and protein. Vitamin C and zinc are not recommended as routine interventions according to some guidelines. Social services need to complete an interview with the resident, if possible, to screen for depression and to help obtain appropriate treatments through the patient’s insurance company or plan, such as beds and dressings. Therapeutic recreation is important in this discussion to ensure that the resident’s psychosocial well-being is maintained, and alternate activities are available if the current ones are not able to be attended to adequately. Nursing is necessary to discuss what changes need to be communicated to the resident, family, and/or provider, as well as maintain a holistic view of the resident.
WHEN OLD/OUTDATED TREATMENTS ARE ORDERED
The need for topical wound care changes as the wound heals or worsens. The use of debridement (wet-to-dry dressings or collagenase) until healed is impossible. These treatments should be used on wounds with slough or eschar until it is removed. At that point, another topical treatment will be needed (J. Black, written communication, September 2018).
In most cases, the wound team recommends topical treatments to the provider. If the wound team is using outdated orders, education must be provided. If your providers are ordering outdated topical treatments, they need to be provided with a list of acceptable orders for the type of wound (Table 1)
DON’S RESPONSIBILITY TO THE WOUND CARE TEAM
The wound care team plays a significant role within a nursing facility, as any skin impairment can require the wound care team. The DON has responsibilities to assist the team with being as effective and resourceful as possible. This includes continuing education, advocating on behalf of the wound care team for new products and services, and ensuring transportation and/or contracts with wound care providers is/are available. If a wound care provider is contracted to the facility, the DON needs to ensure appropriate treatments are done safely and the patient/power of attorney’s right of consent, including refusal of treatment, is obtained and followed.
WHERE TO GET TRAINING FOR WOUND NURSES
While the wound care team is responsible for staying current, the director should offer opportunities to complete continuing education for wound care frequently and on company time, as it is directly related to their job requirements. In an ideal world, there would be money and time to send the wound staff for training. With budget constraints, many hours of continuing education can be obtained at little to no cost by viewing webinars at national organizations (www.npuap.org), manufacturers, and local colleges or universities. The manufacturer’s product representatives should be able to get a list of continuing education opportunities the company provides.
HOW TO KNOW YOUR WOUND NURSE IS DOING THINGS CORRECTLY
At a minimum, the DON should receive a weekly report of all PIs in the facility. This report should include:
1)The date of discovery for each wound.
2)The date of the last change in the treatment plan.
3)If medical interventions are being performed (e.g., sharp debridement).
If any wound is not healed or significantly improved in 6 weeks, the director needs to conduct a chart review to ensure proper care is being provided, including improved nutrition, treatments, and relief of causative agents (pressure). Common problems leading to wound deterioration include:
1) Lying and sitting on the ulcer.
2) Not consuming adequate protein and calories.
3) Using occlusive dressings on necrotic wounds.
The wound cannot heal in the same internal and external environment as when it was created (nutrition, pressure, infection, incontinence, etc.). Everyone on the wound team should examine the wound treatment plan, ask clarifying questions of the larger wound care team about the interventions in place, and make corrections to the treatment plan. For example, sharp debridement is rarely indicated for patients who are receiving hospice care.2 If these steps are taken, families should be notified promptly about the risk of non-healing and should be asked about anticipated interventions (debridement, hospitalization, antibiotics, etc.).
TALKING TO PATIENT AND FAMILY AFTER “IT’S A SIMPLE WOUND, IT WILL HEAL”
The director has the responsibility of oversight of all nursing care provided in the facility. One major component of nursing care is communication between bedside staff, families, and providers. A relatively common occurrence is a change of condition notification to providers and families, but families are told something akin to: “It’s a small, simple wound. It will heal in no time.” Sometime later, the family is asked by a provider for consent for debridement of a necrotic stage 4 PI. The DON should expect complaints, if not litigation, from family members if this is the system for communicating clinical information as it relates to wound care. Families of patients with wounds should expect frequent communication regarding improvement, stagnation, and deterioration of the wound; not just the topical treatment changed. The wound care team may be the best ones to communicate the changes in the wound, but if the team is not doing that often enough, the director should be the one notifying families of these significant wounds. A family member should never walk in and discover a PI for the first time.
F314 TAGS
The Centers for Medicare and Medicaid and the Department of Health and Human Services have determined that avoidable PIs not present upon admission to a facility are a breach to the standard of care and have determined it is an F314 tag.3 Once a PI has been identified, the change in condition must be reported to the provider for treatment options and the power of attorney for the patient. This communication should be taken by the wound care team or DON who can explain the circumstances and plan for treatment and mitigation.
THE TERMINAL ULCER
Ulcers that occur when a resident is at the end of life or on hospice services have very different dynamics than other PIs. The goal for these wounds is not healing but to prevent worsening and educating patients and families on potential outcomes of the wound, such as sepsis. These wounds do not follow the same standard of weekly measurements and curative treatments but are palliated with less frequent dressing changes, lack of unnecessary debridement, and other alterations in care.2The director is responsible for ensuring patients with PIs under hospice care are having goals-of-care discussions regarding wound healing/treatments, advocating for and communicating to providers the patient/family wishes, or preventing unnecessary deterioration in the patient’s quality of life.
CONCLUSION
The DON has a large and dynamic role within the management of chronic wounds, including PIs. This does not encompass all aspects of the DON role but is designed to facilitate understanding and collaboration between the director, the staff, and the providers.
References
1.Skilled Nursing Facility care. Medicare.gov. https://www.medicare.gov/coverage/skilled-nursing-facility-snf-care. Accessed October 4, 2018.
2.Hotaling P, Black J. Ten top tips: palliative wound care. Wounds International. 2018;9(3):16-20.
3.State Operations Manual Appendix PP: Guidance to surveyors for long term care facilities. Rev. 5, 11-19-04. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R5SOM.pdf. Accessed October 4, 2018.