Dr. Robert Snyder is a podiatrist with over 30 years of experience; his practice is limited to wound management and limb preservation. He is Professor and Director of Clinical Research and Fellowship Director at Barry University SPM. Dr. Snyder is certified in foot and ankle surgery by the American Board of Podiatric Surgery and is also a board certified wound specialist. Dr. Snyder is immediate past-president of the Association for the Advancement of Wound Care and past-president of the American Board of Wound Management. In addition to his doctorate, he holds an MSc in Wound Healing and Tissue Repair from Cardiff University. Dr. Snyder has published several book chapters over 125 papers in peer reviewed and trade journals on wound care and has been a principal investigator on more than 30 randomized controlled trials.

Jackson North Surgical Residency Director Assistant Professor of Podiatric Medicine at Barry University

Snyder, Cuffy, Cala and Jafary_Current Dialogues in Wound Management_2017_Volume 3_Issue 1
NOTE: As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual results may vary depending on the patient’s circumstances and condition.
Over the years, varies controversies have been posed regarding the surgical treatment of Charcot Neuropathy (CN). These questions range from what stage of CN one should perform surgery to what type of surgical intervention is indicated for Charcot joint disease. Over the past decade, surgical reconstruction of the Charcot foot and ankle has become more popular because of improved methods of fixation and better overall medical management. Surgical procedures can be categorized as ablative (amputation, drainage, and debridement), curative (exostectomy), and prophylactic/reconstructive (realignment osteotomies, tendon balancing procedures, and arthrodesis).
The indications for surgical reconstruction are marked instability, severe deformity and recurrent ulceration. Acute Charcot deformity in the hind-foot and ankle leads to greater instability than in the mid-foot. Therefore the potential for major complication is higher. The goal of treatment is to provide a stable plantigrade foot with intact skin.
Most patients who develop CN will have adequate arterial inflow to support bone and wound healing. However, patients with suspected vascular disease should undergo vascular evaluation. These patients have multiple medical co-morbidities and should be clinically optimized prior to entertaining surgery.
Understanding these classifications is necessary in surgical planning. Eichenhotz’s landmark monograph is most often used classification. Eihenhotz’s classifying Charcot arthropathy based on radiographic appearance and physiologic. The disease process was classified into 3 separate stages: development, coalescence, and reconstruction.
In recent years, more surgeons have moved from ablative and curative surgeries to reconstructive ones. Internal and external fixation plays a key role. Fixation devices range from simple staples to large diameter screws, intramedullary rods and complex external fixators. Understanding the indications for these modalities will allow for more successful outcomes and fewer complications.
In next section we describe the most common reconstructive techniques including Internal fixation, external fixation and combined internal and external fixation.
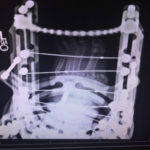
Internal fixation
Recent advances in internal fixation techniques, such as locking plate, solid fixation bolts, and intramedullary beams, have provided encouraging options in patients undergoing surgical management. Internal fixation is best suited for subluxed joints with minimal bony destruction. Good bone quality is essential for screw purchase. It is also preferable to place screws where an intact soft tissue envelope exists. This implies that whenever possible, it is best to perform surgery when plantar ulcerations are healed. Also the presence of osteomyelitis is a contraindicated when it comes to using internal fixation.4 Patients that are unable to maintain non weight-bearing restrictions are not ideal candidates for internal fixation alone and may be supplemented with external fixation. Nevertheless, internal fixation maintains clear advantages over external fixation in that it facilitates compression across joints and buried fixation devices with a single operative procedure.
The intramedullary foot fixation technique (IMFF) spanning the tarsus into the talus and/or calcaneus is a method for addressing unstable midfoot charcot deformity and has various advantages. These advantages include anatomical realignment, minimally invasive fixation technique, formal multiple joint fusion, adjacent joint fixation beyond the level of Charcot collapse, rigid interosseus fixation, and preservation of foot length.
Internal fixation in the acute setting has been attempted, but hardware failure is common, especially if the fragmentation stage has occurred, presumably because of insufficient bone strength and the continuation of deformity.
Figure 1. Internal fixation using beaming technique
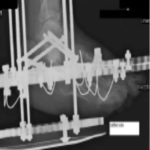
External fixation
Frames are particularly useful in cases in which internal fixation is contraindicated and the patient is facing a major limb amputation. Indications for external fixation include active infection, severe bony deformity, inadequate bone for internal fixation, and ability to use percutaneous approaches and minimal soft tissue dissection in those patients who have a high risk for wound breakdown.
External fixation offers key advantages including; the promotion of stability across several joints; the ability to apply them distant from potentially infected bone; the ability to apply them in the presence of open soft tissue envelope, ability to adjust and manipulate frame after surgery, and early weight bearing to increase healing potential. (Figure 2) One can use dynamic frames such as the Taylor Spatial Frame in the acute phase of Charcot to slowly distract and reduce joint subluxation. Pin tract problems, especially infections, result from micro-motion at the pin-skin interface and the fact that these frames remain in place for as long as three months. As the patient continues through the Charcot stages, consolidation may occur and be held in place with the fixator.
Figure 2. External fixation technique using ring fixation
Combine Internal and external fixation
Combined internal and external fixations allow incorporating the advantages of each technique to provide the best outcome. The surgical planning needs to be precise and many factors have to be considered since it is an invasive procedure. This method usually involves osteotomies with internal fixation, and using external fixation for stronger stabilization. Also internal fixation is used for CN midfoot deformity correction and can be combined with external fixation to address the presence of an equinus associated with Charcot foot.
Morbid obesity, need for soft tissue protection and high risk of hardware failure are some of the reasons for combining internal and external fixation in management of CN deformities.
Figure 3. Internal and external fixation technique using intramedullary screws and Ring fixation
Case Presentation
A 63-year-old male with past medical history significant for NIDDM, Hypertension, and anxiety was admitted to hospital for left foot infection and cellulitis in February 2016. He had been treated by another physician with serial debridement and was told the ultimate treatment would be below the knee amputation.
On clinical examination, he had a rocker bottom foot with equines contracture and a full thickness ulcer to plantar aspect of left foot, with purulence drainage, periwound erythema, warmth and cellulitis of left lower extremity.
Radiograph showed remodeling stages of Charcot deformity severe destruction of Lisfranc joint. Also MRI obtained and a large mass was noted on plantar aspect of left foot where the ulcer was noted. (Figure 4)
Figure 4. Radiograph of left foot showing remodeling stage
Figure 5. Top picture is showing closure of ulcer on plantar aspect of foot. Bottom picture is showing application of external fixator
Figure 6. Two months post operative with external fixation device intact
The goal of surgery was to create an arch and achieve a plantigrade foot and ankle to off-load and prevent ulceration. Surgery was performed by first addressing the equines with performing endoscopic gastrocnemius recession. Next a V-shaped osteotomy with dorsal apex was performed over the Navicular and carried all the way from medial to lateral. Then attention was directed to plantar aspect of foot ulceration where a full thickness ellipse shape incision performed around the ulcer and the soft tissue mass was removed deep to ulcer. Using skin-plasty technique the plantar skin was closed. External fixation frame was used to hold the foot in correct position in attempt to create transverse arch and correcting the deformity. (Figure 5)
In addition to surgery, the psychosocial factors were optimized including obtaining psychiatrist consult to manage anxiety and finding rehab for patient in order to follow up with patient for post operative period. Patient started walking using footplate after 1 month. After 2 months ulcer on plantar aspect showed much improvement and arch presented on plantar aspect of left foot. (Figure 6)
After 3 months external fixation devise removed. Patient was able to walk with CAM boot with completely healed plantar ulcer and sustained and plantigrade foot. (Figure 7)
Conclusion
The actual decision between conservative and surgical intervention depends on assessment of the risks and benefits of each in terms of the deformity present, Comorbidities, The expected recovery time, patient compliance, Psychosocial factors, family and financial support, and many others.
Figure 7. Three months post operative showing completely healed plantar ulcer
The difficulty of structuring a randomized study in a surgical specialty limits the availability of high-level evidence, and the relatively low prevalence of Charcot arthropathy restricts the number of patients per study. Keeping in mind that braceable foot is the goal and not necessary a solid osseous fusion. It is important to look and treat clinically not treating x-ray. Treating x-ray will increase complication rate.
Finally there are many different surgical treatment for CN but the best surgical option for CN patient would depends on 2 main factors: 1- patient’s compliance, 2- The surgeon’s skills to perform the particular type of surgery.
References
1.Shen, W., & Wukich, D. (2013). Orthopaedic Surgery and the Diabetic Charcot Foot. Medical Clinics of North America, 97(5), 873-88
2. doi:10.1016/j.mcna.2013.03.013 2.Lowery, N. J., Woods, J. B., Armstrong, D. G., & Wukich, D. K. (2012). Surgical Management of Charcot Neuroarthropathy of the Foot and Ankle: A Systematic Review. Foot Ankle Int Foot & Ankle International, 33(2), 113-121. doi:10.3113/fai.2012.0113
3.Frykberg, R. (2014). Chapter-10 The Diabetic Charcot Foot: Diagnosis and Management. Contemporary Management of the Diabetic Foot, 78-86. doi:10.5005/jp/books/11997_10
4.Crim, B. E., Lowery, N. J., & Wukich, D. K. (2011). Internal Fixation Techniques for Midfoot Charcot Neuroarthropathy in Patients with Diabetes. Clinics in Podiatric Medicine and Surgery, 28(4), 673-685. doi:10.1016/j.cpm.2011.08.003
5.Pinzur, M. S. (2016). Surgical treatment of the Charcot foot. Diabetes/Metabolism Research and Reviews Diabetes Metab Res Rev, 32, 287-291. doi:10.1002/dmrr.2750
6.Capobianco CM, Stapleton JJ, Zgonis T. The role of an extended medial column arthrodesis for Charcot midfoot neuroarthropathy. Diabet Foot Ankle 2010;1. DOI:10.3402/dfa.v1i0.5282.